Abstract
Background: Cullin 4B(CUL4B) is a member of cullin family, which is a scaffold protein of Cullin-Ring ligase complexes. CUL4B has been reported to be overexpressed in many solid cancers. And evidence supporting the oncogenic role of CUL4B is accumulating, which includes cell proliferation regulation, signal transduction and transcriptional regulation. However, none of them has been reported regarding the expression and biological role of CUL4B in diffuse large B cell lymphoma (DLBCL). We hypothesized that CUL4B could promote tumorigenesis and reduce chemosensitivity by activating autophagy. In this current study, we evaluated the expression and function of CUL4B in DLBCL tissues and cell lines. We also assessed the proliferation and apoptosis of DLBCL cells when treated with a proteasome inhibitor, bortezomib (BZ). The aim of this study is to investigate the functional significance of CUL4B and its therapeutic potential in DLBCL.
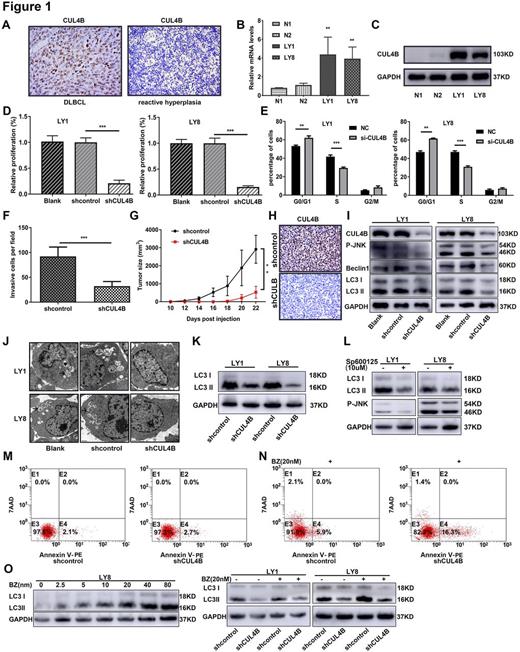
Methods: Immunohistochemistry staining (IHC) for CUL4B expression was performed on tissues of 48 newly diagnosed DLBCL and 30 reactive hyperplasia cases (controls) with informed contents. Peripheral blood mononuclear cells (PBMCs) were isolated from healthy volunteers. Expression levels of CUL4B mRNA and protein in DLBCL cells and PBMCs (controls) were detected by RT-PCR and western blotting. Stable knockdown cell lines were generated by lentiviral infection. Effects of cell viability, cycle and apoptosis were assessed by cell counting kit-8 assay, propidium iodide and Annexin V-PE/7AAD staining, respectively. Invasion ability was analyzed by transwell assay. Autophagosomes were investigated by transmission electron microscopy. ShCUL4B cells and empty lentiviral vectors (shcontrol) cells were subcutaneously injected to SCID-Beige mice to establish enograft models. Animal experiments were performed in accordance with the principles of the Institutional Animal Care.
Results: The positivity of CUL4B was statistically more frequent in DBLCL tissues compared with reactive hyperplasia of lymph nodes tissues (Fig. 1A). Expression of CUL4B was positively correlated with the B symptoms (p=0.043) and Ann Arbor stage of DLBCL patients (p=0.049). CUL4B was also overexpressed in DLBCL cell lines (LY1 and LY8) at both mRNA and protein level (Fig. 1B and C). CUL4B-deletion caused substantial growth suppression in DLBCL cells (Fig.1D). CUL4B interference resulted in an increased accumulation of cells in G1 phase of the cell cycle, with concomitant decreases in the proportion of cells in G2 and S phases compared to control cells (Fig.1E). Moreover, we also found that CUL4B knockdown induced striking reduction in invasion cells (Fig.1F). Furthermore, tumor formation was assessed in xenograft models with CUL4B downregulation. We found that tumor growth was significantly suppressed by CUL4B knockdown (Fig.1G). IHC for CUL4B on xenograft tumor sections showed that tumors derived from shCUL4B cells exhibited significantly lower levels of CUL4B compared to control group (Fig.1H).
To investigate the mechanism of CUL4B promoting tumorigenesis, we further examined whether CUL4B was associated with autophagy. Our data showed that CUL4B silence could significantly reduce autophagy in DLBCL cells (Fig.1I and J). CUL4B silence or JNK inhibitor (Sp600125) caused significantly inhibition of the conversion of LC3-I to LC3-II and reductive phosphorylation of JNK (Fig.1K and L). Our data also demonstrated that the decreased level of autophagy was due to CUL4B modulating in the JNK signaling pathway.
Flow cytometry was performed to evaluate the ability of CUL4B enhancing the drug resistance of BZ in DLBCL cells. No obvious apoptosis occurred with CUL4B-silence (Fig.1M). Interestingly, co-treatment with BZ significantly induced cell apoptosis and inhibited autophagy in the CUL4B-deletion cells (Fig.1N and O). Therefore, we were highly skeptical of the view that CUL4B might suppress the sensitivity of BZ by promoting autophagy in DLBCL.
Conclusions: We confirmed that overexpression of CUL4B contributed to the tumorigenesis and chemo-resistance via activating autophagy in DLBCL. These results have provided a novel biomarker for the pathogenesis and progression of DLBCL. It supports the pursuit of CUL4B as a novel potential target for DLBCL therapy and prevention for chemotherapy resistance.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal